What are the types of cancer research?
In any battle, knowing and understanding your adversary is crucial. This is true for our fight against cancer as well, and research is the key to our combat strategy. Cancer research plays a vital role in gaining insights into the nature of the disease. Through systematic investigation and the creation of new knowledge, we can enhance our understanding of cancer. Armed with this knowledge, we can then develop more effective strategies for the prevention and treatment of cancer.
Researchers study every stage of the cancer journey, from causes (called etiology) and prevention to screening, diagnosis, and treatment (therapy) as well as survivorship and quality-of-life (palliative) care. This is called the cancer continuum.
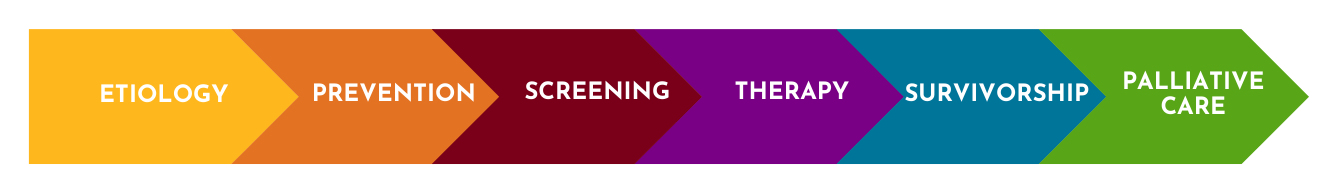
What we know about cancer—how to reduce cancer risk, how it develops, how to treat it, and how to help people cope with it—all depends on different types of research and what is discovered as a result.
The Masonic Cancer Center, University of Minnesota, is a community of more than 600 researchers who study cancer. The things they study are broken down into six research areas that are organized around specific themes spanning the cancer continuum. The programs interact with one another and with groups throughout the world to uncover better ways to treat and prevent cancer. These six areas, and the portions of the cancer continuum they span, are shown below.
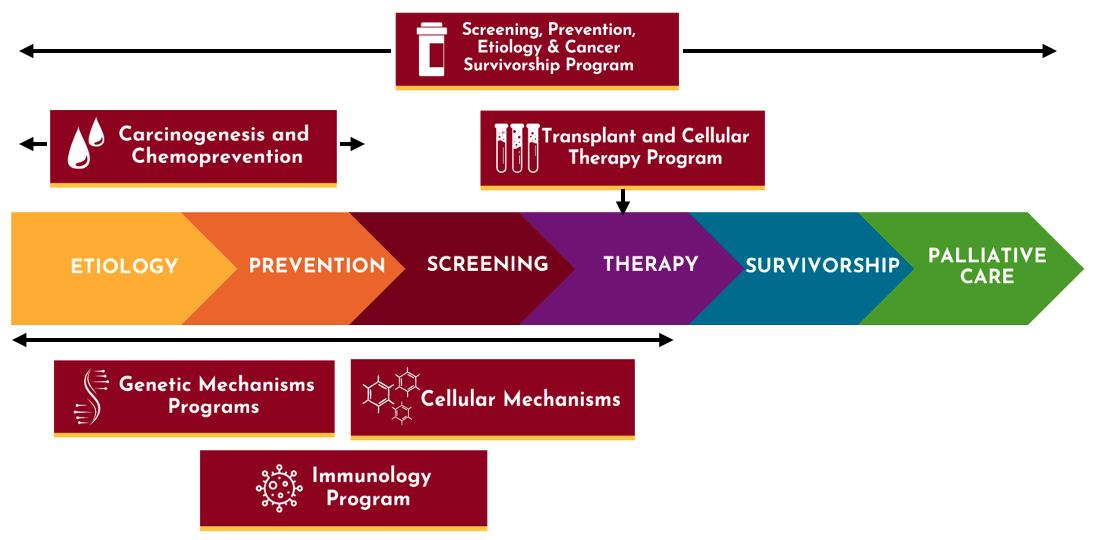
Within these research programs, MCC scientists conduct research at different levels and settings. We use these different levels and settings to group cancer research into four main types: basic, clinical, population-based, and translational. Below, we take a closer look at each of the four types.

Basic research

The first level of research is called basic research, also known as laboratory research or bench science. Basic researchers study the cells, molecules, and genes that are the building blocks of life, working to understand how healthy cells grow and then identifying the differences between those healthy cells and cancer cells.
This approach allows researchers to control and test for many different factors, for example, turning specific genes on or off, or exposing cells to a specific substance, condition, or possible treatment—and then measuring the effects of whatever is tested. Researchers can even use the cells from healthy volunteers to do this testing—and the volunteers definitely don’t have to be human. Cells from animals like mice, or even lab grown cells, are commonly used in cancer research.
After finding a promising idea that works in cells, researchers need to take that idea to the next level. But, it’s not safe or practical to move directly from cells to people. That’s where animal research comes into play—because animal models have certain similarities to humans, researchers can carry out and repeat important experiments that would be practically or ethically impossible to test initially in people. Scientists will often use mice, fruit flies, or even zebrafish to try out an idea, test, or treatment!
Findings from laboratory, or basic, research are an essential starting point for informing future tests and treatments. However, even the best lab research has its limitations. That’s because humans are complex creatures, and no animal model can perfectly predict how a specific type of cancer will progress, or how a particular treatment will work in patients. This is where another level of research, translational research, becomes crucial. We’ll tackle translational research a bit later in this blog.
Translational research

During translational research, researchers take what they have learned in the lab and apply it in patient care. The knowledge gained from this work then goes back to the lab to inform even further investigations. Many people say that translational research “bridges the gap” between basic and clinical research by bringing together a number of different specialists to refine and advance the application of a discovery.
Translational research seeks to produce more meaningful, applicable results that directly benefit human health—in other words, that directly benefit patients. The goal of translational research is to move basic science discoveries into practice with patients more quickly and efficiently.
Masonic Cancer Center researchers play a key role in designing and developing medicines that inform future treatment strategies, thanks in large part to our Cancer Research Translational Initiative (CRTI). For example, CRTI has facilitated the translation of TriKE GTB-3550—a cancer therapy that uses special killer cells to attack cancer cells—led by MCC’s Dr. Jeff Miller. The first generation TriKE, or the initial design, was developed to study its effects on a specific set of drug-resistant leukemias in a first-in-human trial led by Dr. Mark Juckett. Thanks to that trial, MCC’s Dr. Martin Felices and team developed a more potent second-generation TriKE, and MCC’s Dr. Nicholas Zorko and team have used lessons from this process to create a third special TriKE dedicated to examining the response of drug-resistant solid tumors such as prostate cancer and sarcoma.
And the benefits of translational research don’t stop with patients—this research provides a crucial pivot point after clinical trials are conducted as well. That’s because researchers can explore how the trial’s resulting treatment or guidelines can be implemented by physicians in their practice. And, the clinical outcomes might also motivate basic researchers to re-evaluate their original assumptions or find new things to test that their original research hadn’t yet explored.
Clinical research

In clinical research, promising treatments or tools are carefully studied in people. Clinical research studies, also known as clinical trials, explore whether new treatments, medications, and diagnostic techniques are safe and effective.
Clinical research includes more than new drug development—it can be used to test anything that helps prevent, find, predict, treat, or manage cancer. That could include testing a phone app to monitor symptoms, an exercise program to help patients stay active, or a questionnaire to help doctors and nurses monitor potential health issues like pain.
Clinical research is a critical step in the research pipeline because it ensures that what is being tested is safe and will work well for large groups of people. Clinical trials are often designed to learn if a new treatment is more effective or has less harmful side effects than existing treatments. At MCC, our Clinical Trials Office (CTO) tackles this process in partnership with physician researchers. The CTO is a large team of cancer center professionals who are dedicated to meeting the needs of researchers and their patients by providing exceptional trial management services. Clinical research teams prioritize patient safety, and are focused on ensuring the highest level of data integrity and regulatory compliance.
Today’s clinical trials often become tomorrow’s new standard of care, boosting many patients' quality of life now, and helping ensure that future patients have continuously higher standards of care. Participation in a clinical trial provides qualified patients with early access to cutting-edge therapies. Rigorous regulatory standards ensure that patient care while on these trials is as good and often better than standard treatments.
Want to read more about clinical trials and the phases they go through? Check out our explainer blog to learn more about clinical trials and why they’re so important.
Population-based research

While cancer affects all population groups, studies show it often has a larger or more severe impact on some groups over others. So, understanding and addressing these health disparities is crucial.
Population-based research explores the causes of cancer, cancer trends, and factors that affect the delivery and outcomes of cancer care in specific populations. This field of cancer research brings together scientists whose research focuses on cancer prevention, early detection, health outcomes, and how to best share with people, especially diverse communities, the information uncovered.
Many of our researchers focus on cancer risks for vulnerable populations—children, people with severe mental illness, medically-underserved communities, and patients from across Greater Minnesota who are geographically isolated due to cost of treatment and long travel distances. This is evidenced by initiatives like the 10,000 Families Study, a study of family health in Minnesota that invites families from across the state to participate over time with the purpose of understanding the influences of genetics, lifestyle, and environment on health and illness, including cancer.
At the end of the day, the reason our scientists and doctors are able to provide the most cutting-edge cancer treatments, prevention education, and diagnosis tools is because all of these types of research—from the very beginning stages in a lab all the way to the clinic—work together. Solving the problem of cancer is a collaborative effort, and we’re proud and humbled to have such a strong legacy of support from partners, community members, and beyond to continue writing cancer’s last chapter.
Want to get updates on what our researchers and doctors are up to? Sign up today for our Community Matters e-newsletter to receive a monthly round-up of MCC’s top stories and events. And, if you’re looking for education and training opportunities, get on the list for Career Connections, a monthly collection of all career-related offerings at the cancer center.