Digging Deeper Into Breast Cancer Prevention and Screening with Dr. Damé Idossa
Breast cancer is among the top five causes of death in Minnesota Women. Of those, black women have a 40 percent higher mortality rate than white women when it comes to breast cancer. It is extremely important that we work to close this gap and understand how we can improve outcomes for women with breast cancer.
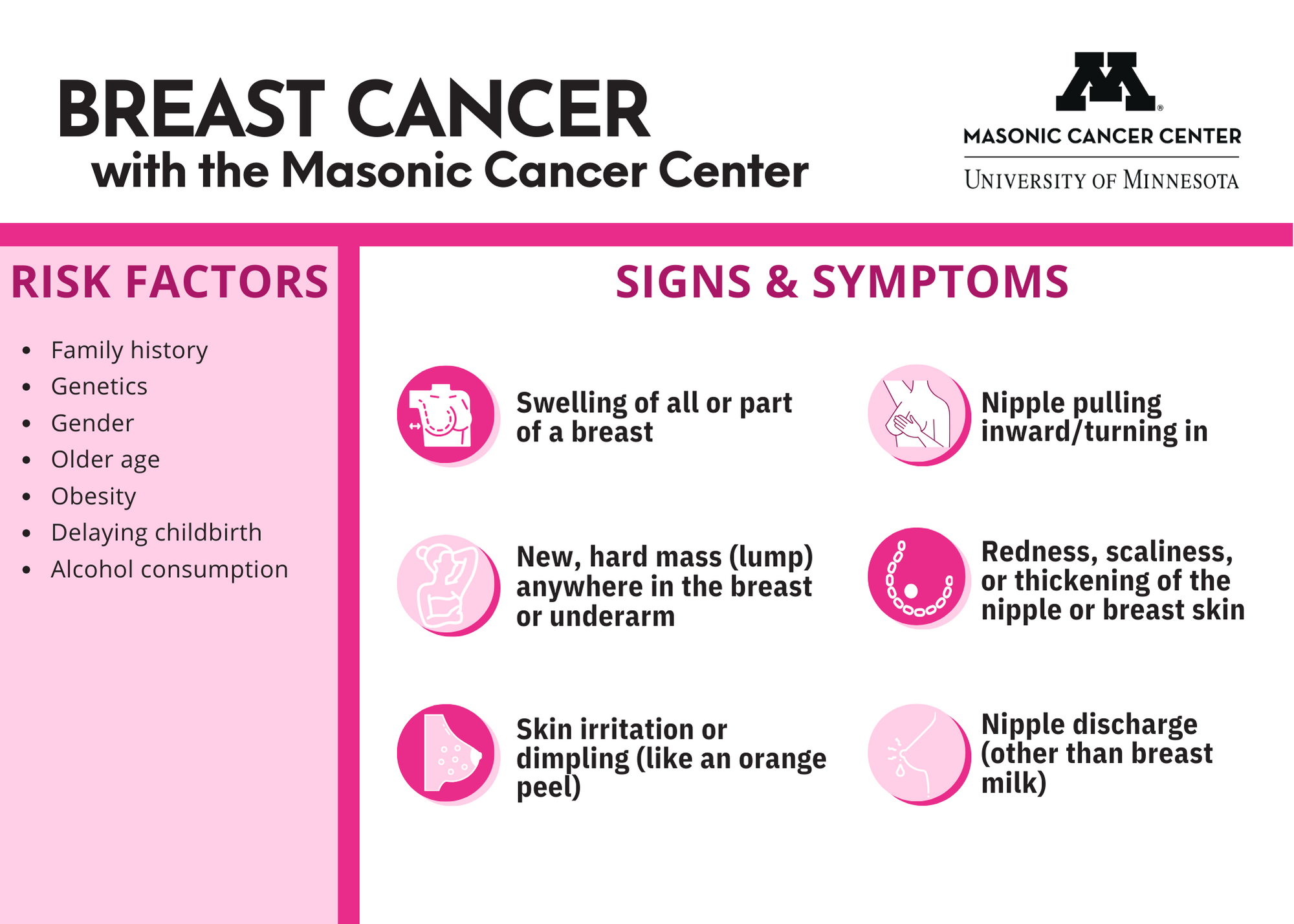
For Breast Cancer Awareness Month this October, Damé Idossa, MD, an assistant professor of medicine at the University of Minnesota Medical School and member of the Masonic Cancer Center, talks about health disparities within breast cancer, closing the gaps, and the importance of screening. Before jumping in, check out the infographic below for insight into additional screening and prevention guidelines.
Could you give us some background on growing up, your education, and what brought you back to Minnesota?
I was born in Ethiopia and immigrated to Minneapolis when I was 8 years old. I grew up in Richfield, Minnesota and then went to the University of Minnesota for undergrad where I majored in biology and physiology. I attended Yale University for medical school. After that, I came back to Minnesota and did internal medicine residency at the Mayo Clinic. I completed my oncology fellowship training at UCSF in California and now I am back at the University of Minnesota working primarily in breast cancer.
How did you know you wanted to work in medicine - specifically breast cancer?
Medicine was always a contender among a few other things that I was potentially interested in. I’ve always had an interest in the sciences and really enjoyed that aspect throughout my undergraduate training. I was involved in a pipeline program at the University of Minnesota called “Minnesota’s Future Doctors” program which really exposed me to medicine and research, and also gave me the opportunity to imagine what a career in medicine would be like. After that program, I was confident that I would be pursuing a career in medicine.
As for oncology, I didn’t decide on that until I was in residency. I think sometimes when people think of oncology, they think it is always really sad, but that’s not always the case, there are many moments of joy. In residency, I had the opportunity to see what the inpatient practice would be like, which at times can be challenging, but I also had the opportunity to work in the outpatient setting where patients were living for many many years, which was really gratifying to see. I was able to see the longitudinal relationships that oncologists can have with their patients and also the huge difference that the researchers and physicians were making in people’s lives. That was when I really decided on oncology.
My interest in breast cancer didn’t come until my fellowship program. I trained with some of the world’s leading breast oncologists, so that was a really driving force. I’ve always been interested in women’s health, and I think that breast cancer really encompasses that as well.
Why did you choose to come back to the University of Minnesota?
I would say it’s for two reasons: One is family. All of my immediate family is in Minnesota and I wanted to be closer to them. Secondly, it was the community here in Minneapolis. I’m really interested in working with diverse and immigrant populations. One of my major research interests is within the realm of health equity and health disparities. For example, there are many issues within immigrant communities in terms of cancer screenings. It’s a community that needs a lot of support and there’s a lot of work to do in that space.
Additionally, I think you have to find your people wherever you go. Within each institution I’ve worked at I ask myself, “Are these the folks that I would work well with?” And as I was going through each interview process, that was a question I kept asking myself. The colleagues that I work closely with here in breast cancer are all fantastic.
What comes to mind when you think about Breast Cancer Awareness Month
Breast cancer is a cancer that we, as researchers and physicians, have made a lot of headway in, in terms of survival rates. Most of our patients actually do really well long-term, but, if you look at the data a little bit closer, that's not the case for everyone. There are unfortunately many disparities that still exist with regards to breast cancer outcomes. There are many different reasons as to why those disparities exist, and it’s not something that we all think about. For example, when we look at breast cancer mortality, Black women have a 40% higher mortality rate compared to white women. I think about those things quite a lot. And many researchers are working towards figuring out how to close that gap.
Here in Minnesota, what do you think are the most impactful breast cancer prevention methods?
One issue in Minnesota is disparities within breast cancer screening. In other parts of the country, Black women have very comparable breast cancer screening rates to white women, but their outcomes are still worse. There are also screening gaps between women who live in rural areas compared to urban areas. I think for our communities in Minnesota, we can focus on screening as one of the preventative measures we can take to reduce disparities. This not only means ensuring people have access to getting screening mammograms, but also that they can get time off work, have transportation, have childcare, etc. Ensuring that all of the social needs that people might have are addressed in order to allow them to actually engage in their care and stay up-to-date with their screenings is really important.
Are there services available in the community that could help fill the gaps for people to more easily access screenings and other types of care?
One of the two organizations I’ve learned about recently that I think is doing really great work is the Breast Cancer Gaps Project. They really focus on the disparities I mentioned earlier in Black women, and their whole aim is to increase screening rates in Black women in Minnesota. The other group is Gilda’s Club. They do really great work and would be a helpful organization to be aware of. There are many other organizations that I am still learning about.
What is happening at the University of Minnesota in either cancer research or care that excites you about being here?
From a research standpoint, we have many amazing clinicians and researchers who are doing really exciting work in breast cancer. We also have many clinical trials available at the University of Minnesota that provide patients with innovative treatment options for their cancer. One example of this is a trial called the I-SPY clinical trial, which is something called an “adaptive randomized trial” that allows us to test many different treatments for breast cancer and selects the ones that should work best for our patients based on the molecular subtypes of their breast cancer. It is really a way to personalize treatment options and tailor the right treatment for each patient.
From a care standpoint, I love the ability to allow patients to see a specialist here at the University of Minnesota but get their care closer to home if they desire. For a lot of patients, it can be a huge barrier to get onsite, pay for parking, take time off work, and navigate the clinic. If you can still have access to a specialist at the University but get your infusions locally—closer to where you actually live—that’s huge. That is something I have been really impressed with.
What does it mean to you to be able to serve a diverse community as a physician of color? How would you describe the importance of representation in medicine?
I’ve certainly come full circle. I’m coming back to the place where I was initially introduced to medicine as a prospective career. Within oncology, Black women make up less than 2% of physicians. There aren’t very many of us, so to be able to be in a place where other students and trainees can see someone that looks like them as an oncologist is an honor. In addition, that means people in the community also see physicians that look like them and can potentially speak their language. For me, that is huge. For the students and trainees, I want to ensure that the door stays open so that they can walk this same path if they desire. And for patients, I think it’s an opportunity to break barriers that exist for patients of color and build trust with them so that they can access the care they deserve and hopefully end up having better outcomes. Thinking about the possibility of all of that is really exciting and I’m really grateful for the opportunity.
How do you think younger women can be proactive in their own breast health as well as with the other women in their lives?
It’s now well known that cancer screening dramatically dropped during the pandemic. After that, some populations never really got back to their baseline for regular screenings. There are many people who have missed or delayed their screening over the past few years. I think it’s especially important for those who are 40 years old and above to get screened. Depending on family history or genetics, some people may need to get screening earlier than that. For those who are younger than 40 and don’t have a family history of breast cancer, it’s always important to be mindful and recognize changes in their body. If they notice any new breast lumps, skin changes, or anything else that concerns them, they should get checked out. We unfortunately see breast cancer in young women, even when they don’t have a family history. So it’s important to stay vigilant and advocate for themselves.
Your generous gift could be transformational. Help power our breast cancer research by making a gift today.
